Automated Classification of Multi-Class Human Protozoan Parasites using Xception as Transfer Learning
Keywords:
Protozoan, Parasites, Transfer Learning, Xception OptimizerAbstract
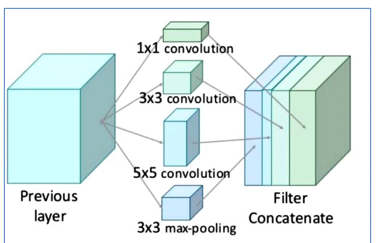
Infections caused by protozoan parasites can cause serious health problems. Malaria infection is an infection with the most recorded infection cases in the world as reported by World Health Organizer (WHO) which has reported cases of Malaria infection in 2020 experienced a significant increase from the previous year. There were 241 million global cases, which previously recorded 227 million global cases. Apart from Malaria, there are still many cases caused by other protozoan parasites such as Babesia, Leishmania, Toxoplasma, Trichomonad, and Trypanosome who identified in this study. Therefore, it is necessary to use technology that can help microscopic experts to diagnose in a fast time and with optimal results. Using the Transfer Learning method with Xception architecture can produce optimal accuracy. In the research in this paper, we use four different optimizers including Adam, RMSprop, SGD, and Adadelta as comparisons with each other. Of the four optimizers, the most optimal result in this study is Adam optimizer with an accuracy of 97%. Therefore, the methodology that we use can help classify the types of protozoan parasites which can make the process faster and can reduce costs in the identification process.
Downloads
References
E. Texeira, V. Morais, M. Rodriguez, and N. Suárez, “Respiratory Tract Infections: Parasites,” in Encyclopedia of Infection and Immunity, Elsevier, 2022, pp. 27–31. doi: 10.1016/B978-0-12-818731-9.00118-X.
A. Martínez-Flórez et al., “Repurposing bioenergetic modulators against protozoan parasites responsible for tropical diseases,” Int. J. Parasitol. Drugs Drug Resist., vol. 14, pp. 17–27, Dec. 2020, doi: 10.1016/j.ijpddr.2020.07.002.
Y. Shi et al., “COVID-19 pharmacological research trends: a bibliometric analysis,” Intell. Med., 2023, doi: 10.1016/j.imed.2022.06.004.
“World malaria report,” 2021. https://www.who.int/publications-detail-redirect/9789240040496
S. Arifin, H. Garminia, and P. Astuti, “Dimensi Valuasi dari Daerah Ideal Utama,” Pros. Semnas KPA Univ. Sanata Dharma, pp. 9–16, 2016.
S. Momčilović, C. Cantacessi, V. Arsić-Arsenijević, D. Otranto, and S. Tasić-Otašević, “Rapid diagnosis of parasitic diseases: current scenario and future needs,” Clin. Microbiol. Infect., vol. 25, no. 3, pp. 290–309, Mar. 2019, doi: 10.1016/j.cmi.2018.04.028.
E. Charpentier et al., “Performance evaluation of different strategies based on microscopy techniques, rapid diagnostic test and molecular loop-mediated isothermal amplification assay for the diagnosis of imported malaria,” Clin. Microbiol. Infect., vol. 26, no. 1, pp. 115–121, Jan. 2020, doi: 10.1016/j.cmi.2019.05.010.
N. Singla and V. Srivastava, “Deep learning enabled multi-wavelength spatial coherence microscope for the classification of malaria-infected stages with limited labelled data size,” Opt. Laser Technol., vol. 130, p. 106335, Oct. 2020, doi: 10.1016/j.optlastec.2020.106335.
I. B. I. B. Muktyas, Sulistiawati, and S. Arifin, “Digital image encryption algorithm through unimodular matrix and logistic map using Python,” in AIP Conference Proceedings, Apr. 2021, vol. 2331. doi: 10.1063/5.0041653.
K. Qu, F. Guo, X. Liu, Y. Lin, and Q. Zou, “Application of Machine Learning in Microbiology,” Front. Microbiol., vol. 10, Apr. 2019, doi: 10.3389/fmicb.2019.00827.
D. Banerjee and T. D. Sparks, “Comparing transfer learning to feature optimization in microstructure classification,” iScience, vol. 25, no. 2, p. 103774, Feb. 2022, doi: 10.1016/j.isci.2022.103774.
P. Thirumalaraju et al., “Evaluation of deep convolutional neural networks in classifying human embryo images based on their morphological quality,” Heliyon, vol. 7, no. 2, p. e06298, Feb. 2021, doi: 10.1016/j.heliyon.2021.e06298.
Hidayaturrahman, E. Dave, D. Suhartono, and A. M. Arymurthy, “Enhancing argumentation component classification using contextual language model,” J. Big Data, vol. 8, no. 1, p. 103, 2021, doi: 10.1186/s40537-021-00490-2.
L. MacNeil, S. Missan, J. Luo, T. Trappenberg, and J. LaRoche, “Plankton classification with high-throughput submersible holographic microscopy and transfer learning,” BMC Ecol. Evol., vol. 21, no. 1, p. 123, Dec. 2021, doi: 10.1186/s12862-021-01839-0.
A. Adel, M. M. Soliman, N. E. M. Khalifa, and K. Mostafa, “Automatic Classification of Retinal Eye Diseases from Optical Coherence Tomography using Transfer Learning,” in 2020 16th International Computer Engineering Conference (ICENCO), Dec. 2020, pp. 37–42. doi: 10.1109/ICENCO49778.2020.9357324.
S. More and J. Singla, “A generalized deep learning framework for automatic rheumatoid arthritis severity grading,” J. Intell. Fuzzy Syst., vol. 41, no. 6, pp. 7603–7614, 2021, doi: 10.3233/JIFS-212015.
K. Sriporn, C.-F. Tsai, C.-E. Tsai, and P. Wang, “Analyzing Malaria Disease Using Effective Deep Learning Approach,” Diagnostics, vol. 10, no. 10, p. 744, Sep. 2020, doi: 10.3390/diagnostics10100744.
C.-H. Su, P.-C. Chung, S.-F. Lin, H.-W. Tsai, T.-L. Yang, and Y.-C. Su, “Multi-Scale Attention Convolutional Network for Masson Stained Bile Duct Segmentation from Liver Pathology Images,” Sensors, vol. 22, no. 7, 2022, doi: 10.3390/s22072679.
A. S. B. Reddy and D. S. Juliet, “Transfer learning with ResNet-50 for malaria cell-image classification,” in 2019 International Conference on Communication and Signal Processing (ICCSP), 2019, pp. 945–949.
D. Setyawan, R. Wardoyo, M. E. Wibowo, E. E. H. Murhandarwati, and J. Jamilah, “Malaria classification using convolutional neural network: a review,” in 2021 Sixth International Conference on Informatics and Computing (ICIC), 2021, pp. 1–9.
I. LAHSAINI, M. EL HABIB DAHO, and M. A. CHIKH, “Deep transfer learning based classification model for covid-19 using chest CT-scans,” Pattern Recognit. Lett., vol. 152, pp. 122–128, Dec. 2021, doi: 10.1016/j.patrec.2021.08.035.
M. Usharani, B. Sakthivel, S. Gayathri Priya, T. Nagalakshmi, and J. Shirisha, “An Optimized Deep-Learning-Based Low Power Approximate Multiplier Design,” Comput. Syst. Sci. Eng., vol. 44, no. 2, pp. 1647–1657, 2023, doi: 10.32604/csse.2023.027744.
R. Zoetmulder, E. Gavves, M. Caan, and H. Marquering, “Domain- and task-specific transfer learning for medical segmentation tasks,” Comput. Methods Programs Biomed., vol. 214, p. 106539, Feb. 2022, doi: 10.1016/j.cmpb.2021.106539.
B. Nigam, A. Nigam, R. Jain, S. Dodia, N. Arora, and B. Annappa, “COVID-19: Automatic detection from X-ray images by utilizing deep learning methods,” Expert Syst. Appl., vol. 176, p. 114883, Aug. 2021, doi: 10.1016/j.eswa.2021.114883.
N. Das, E. Hussain, and L. B. Mahanta, “Automated classification of cells into multiple classes in epithelial tissue of oral squamous cell carcinoma using transfer learning and convolutional neural network,” Neural Networks, vol. 128, pp. 47–60, Aug. 2020, doi: 10.1016/j.neunet.2020.05.003.
S. Showkat and S. Qureshi, “Efficacy of Transfer Learning-based ResNet models in Chest X-ray image classification for detecting COVID-19 Pneumonia,” Chemom. Intell. Lab. Syst., vol. 224, p. 104534, May 2022, doi: 10.1016/j.chemolab.2022.104534.
A. Manickam, J. Jiang, Y. Zhou, A. Sagar, R. Soundrapandiyan, and R. Dinesh Jackson Samuel, “Automated pneumonia detection on chest X-ray images: A deep learning approach with different optimizers and transfer learning architectures,” Measurement, vol. 184, p. 109953, Nov. 2021, doi: 10.1016/j.measurement.2021.109953.
M. Gour and S. Jain, “Automated COVID-19 detection from X-ray and CT images with stacked ensemble convolutional neural network,” Biocybern. Biomed. Eng., vol. 42, no. 1, pp. 27–41, Jan. 2022, doi: 10.1016/j.bbe.2021.12.001.
S. Arifin et al., “Graph Coloring Program of Exam Scheduling Modeling Based on Bitwise Coloring Algorithm Using Python,” 2022, doi: 10.3844/jcssp.2022.26.32.
W. F. Al Maki, I. B. Muktyas, S. Arifin, Suwarno, and M. K. B. M. Aziz, “Implementation of a Logistic Map to Calculate the Bits Required for Digital Image Steganography Using the Least Significant Bit (LSB) Method,” J. Comput. Sci., vol. 19, no. 6, pp. 686–693, 2023.
Downloads
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
All papers should be submitted electronically. All submitted manuscripts must be original work that is not under submission at another journal or under consideration for publication in another form, such as a monograph or chapter of a book. Authors of submitted papers are obligated not to submit their paper for publication elsewhere until an editorial decision is rendered on their submission. Further, authors of accepted papers are prohibited from publishing the results in other publications that appear before the paper is published in the Journal unless they receive approval for doing so from the Editor-In-Chief.
IJISAE open access articles are licensed under a Creative Commons Attribution-ShareAlike 4.0 International License. This license lets the audience to give appropriate credit, provide a link to the license, and indicate if changes were made and if they remix, transform, or build upon the material, they must distribute contributions under the same license as the original.